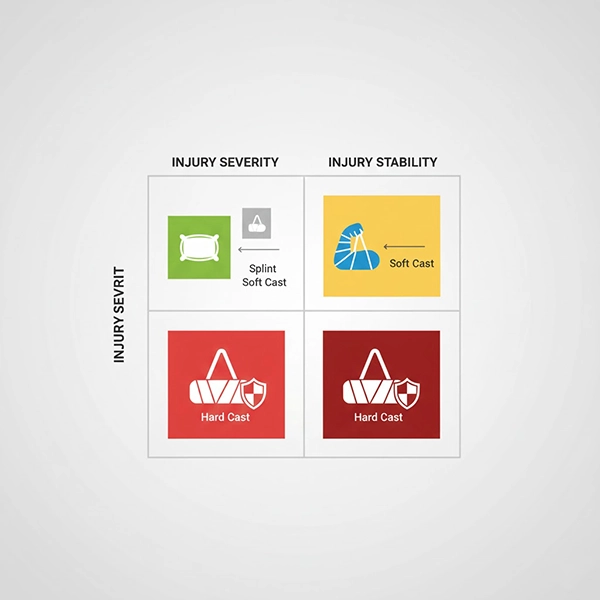
A soft cast cures semi-rigid, preserving slight flexibility while providing supportive immobilization. It suits scenarios where full rigidity isn’t necessary and controlled motion plus easier skin/edema monitoring are desired. Below are practical indications, decision criteria, and semi-rigid protocols.
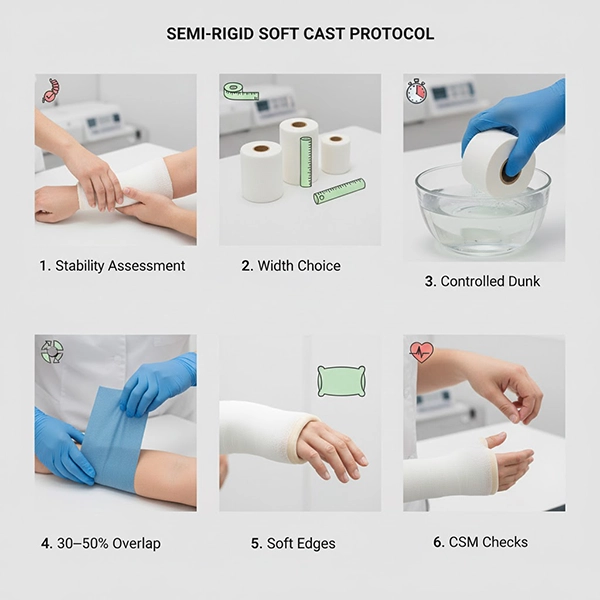

When clinical stability aligns with the need for comfort, breathability, and graded rehab, a soft cast offers the best balance. For tailored protocols and staff training, please contact our team.