Combining Fiberglass with Bioactive Materials to Enhance Bone Healing
Fiberglass orthopedic casting tapes are valued for high strength, low weight, and radiolucency. A next step is integrating bioactive materials—such as hydroxyapatite (HA), bioactive glass, and controlled-release agents—so that the cast offers not only mechanical immobilization but also a bio-supportive microenvironment around the fracture. This article outlines principles, benefits, challenges, and potential clinical pathways of fiberglass casting tape combined with bioactive components.

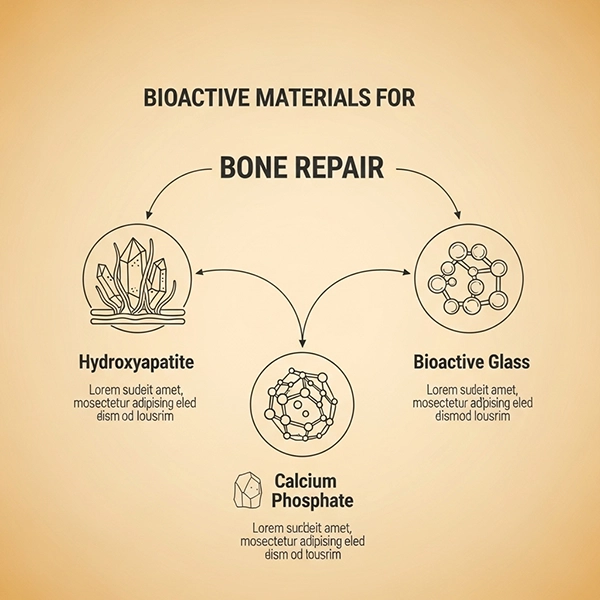
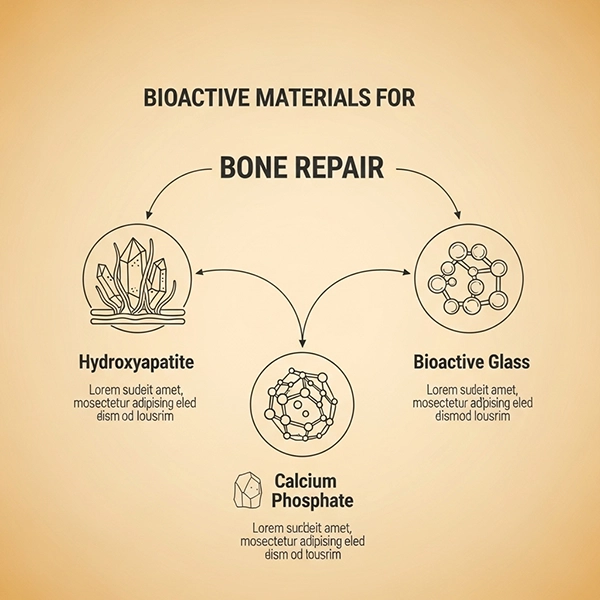
What Are Bioactive Materials & Why They Matter
Hydroxyapatite mimics bone mineral and promotes osteoconduction. Bioactive glasses release ions (e.g., Ca, P, Si) that foster an apatite layer and cell attachment. Calcium phosphates (e.g., TCP) can resorb while new bone forms. Integrating these into fiberglass casts aims to augment healing biology alongside mechanical stability.
Mechanisms for Enhancing Bone Repair
- Improved interfacial osteogenesis: HA/BG coatings enhance protein adsorption and cell adhesion.
- Beneficial ion release: Bioactive glass modulates osteogenic signaling via local ionic cues.
- Local controlled delivery: Micro/nanocapsules can provide anti-inflammatory or antimicrobial agents.

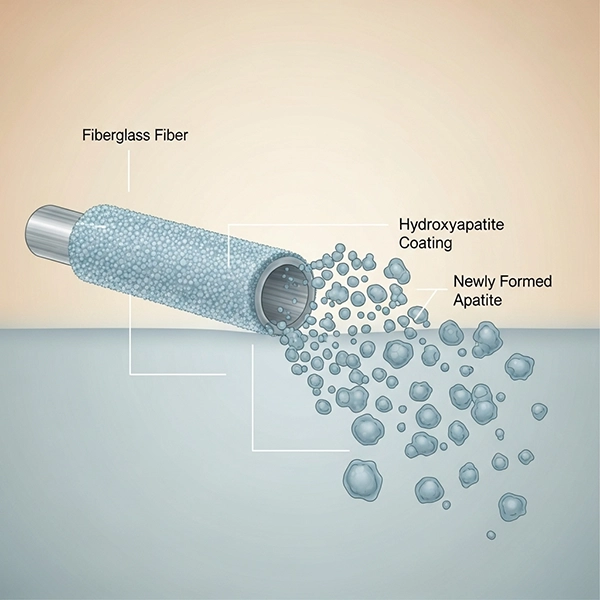
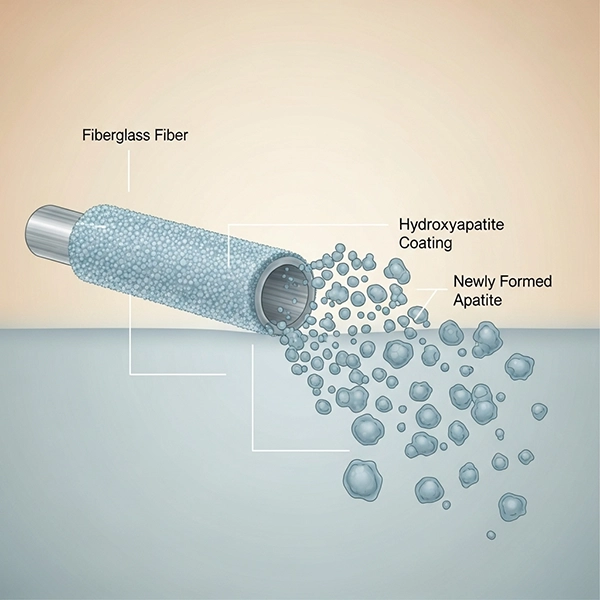
Integration Strategies with Fiberglass
- Surface coatings on fibers: Thin HA/BG layers to boost bioactivity without compromising breathability.
- Resin-loaded bioactive fillers: Mixing HA/BG powders into the water-activated resin; control viscosity and dispersion.
- Interlayer inserts: Placing thin bioactive sheets between cast layers for targeted contact.
- Micro/nanocapsules: On-demand release of antimicrobials/anti-inflammatories during early stages.
Benefits & Clinical Opportunities
- Dual mechanical–biological support at the fracture site.
- Preserved radiolucency when bioactive loading is chosen judiciously; better follow-up imaging than POP.
- Potential infection risk mitigation via local antimicrobial delivery—pending robust validation.
Challenges & Safety Considerations
- Property trade-offs: Excess filler can affect layer molding and porosity.
- Release kinetics: Dose and profiles must be carefully engineered and tested.
- Regulatory path: ISO 10993 biocompatibility, sterilization stability, and clinical evidence are mandatory.
Selection & Use Guidance
- For delayed-healing risk profiles, HA/BG-integrated designs are a promising R&D direction.
- Use proper undercast padding for sensitive skin; manage direct contact with active fillers.
- Storage: 15–30°C, RH < 60%; rolls should feel pliable; respect expiry for consistent performance.
Conclusion & CTA
By combining fiberglass casts with bioactive components, future immobilization may evolve from purely mechanical to bio-intelligent support of bone repair. For technical evaluation, sourcing high-quality synthetic cast bandages, and co-developing bioactive options, visit our product page.